Top 17 reasons why telehealth works best for patients and doctors
Healthline • November 17, 2020
Top 17 reasons why telehealth works best for patients and doctors

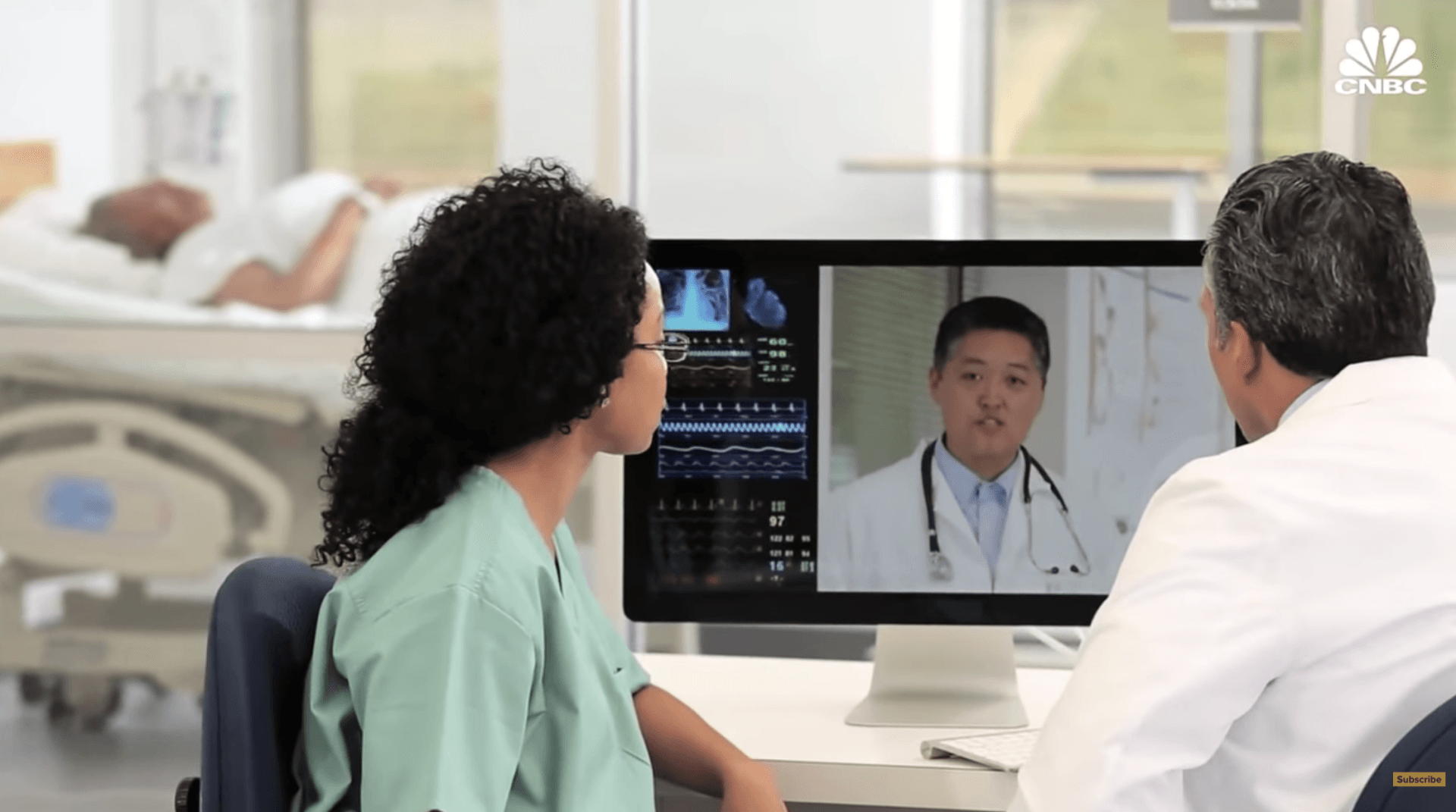
Telemedicine is the ability of healthcare providers to meet with patients remotely via telephone or video.
This practice has been around almost as long as telephones but has become more popular and practical during the COVID-19 pandemic.
Improvements in technology and changes to insurance reimbursement rulings have helped increase the acceptance of telemedicine. Without it, doctors and therapists wouldn’t be able to connect with patients as easily, especially during the pandemic.
As telemedicine has become widespread, professionals and patients have grown more comfortable connecting virtually.
Benefits
Telemedicine isn’t meant to take the place of face-to-face visits. While it does have some disadvantages, which we’ll get into later, its benefits are undeniable.
They include:
1. Easy access to specialists
Not everyone has an ongoing relationship with a doctor they can call when they need one. Many online medical networks offer round-the-clock access to all kinds of specialists, without an appointment, at any time of day or night.
2. Lower cost
Doctors and therapists can be expensive, even for people with good health insurance. Telemedicine appointments typically cost less than in-person visits do. This reduces out-of-pocket costs, removing a barrier to care.
3. Medical access for people without health insurance
Not having adequate health insurance can be an obstacle to seeing a doctor. Many online companies provide cash-pay telemedicine, which doesn’t require health insurance or referrals.
4. Medical access for people in rural areas
Country living has many benefits, but fast access to medical care isn’t always one of them. For people who live many miles from the nearest medical facility, telemedicine provides a way to meet with a doctor quickly.
This saves time and allows people to stay off the road when driving conditions are less than optimal, such as during a snowstorm or hailstorm.
5. Medical access for people in underserved urban areas
The trend of hospital closures in inner-city neighborhoods has affected thousands of Americans, especially communities of color and people without health insurance.
Telemedicine helps break this cycle by providing a way for people to see a doctor before they get extremely sick.
6. Reduced exposure to pathogens
Hours-long waits in doctors’ waiting rooms with other patients can contribute to the spread of COVID-19, the flu, and other viruses. Telehealth keeps patients at home, avoiding exposure to viruses and germs. This helps protect medical professionals as well.
7. Middle-of-the-night care for babies and children
Babies have a knack for spiking fevers or getting sick in the middle of the night. Rather than rely on an internet search, parents can use telehealth services to connect quickly with doctors who can give answers and provide a diagnosis, and even a prescription, when needed.
8. No need for childcare
Parents get sick, too, and it can be challenging to take little ones along to a doctor’s visit. Telehealth eliminates this need, as well as the additional cost of childcare.
9. Doctors get to stay home too
During the pandemic, many medical offices have closed or reduced their hours. Cybersecurity tools such as virtual private networks have enabled doctors and therapists to treat patients safely from their home offices. This access also allows doctors and patients to connect after hours and on weekends.

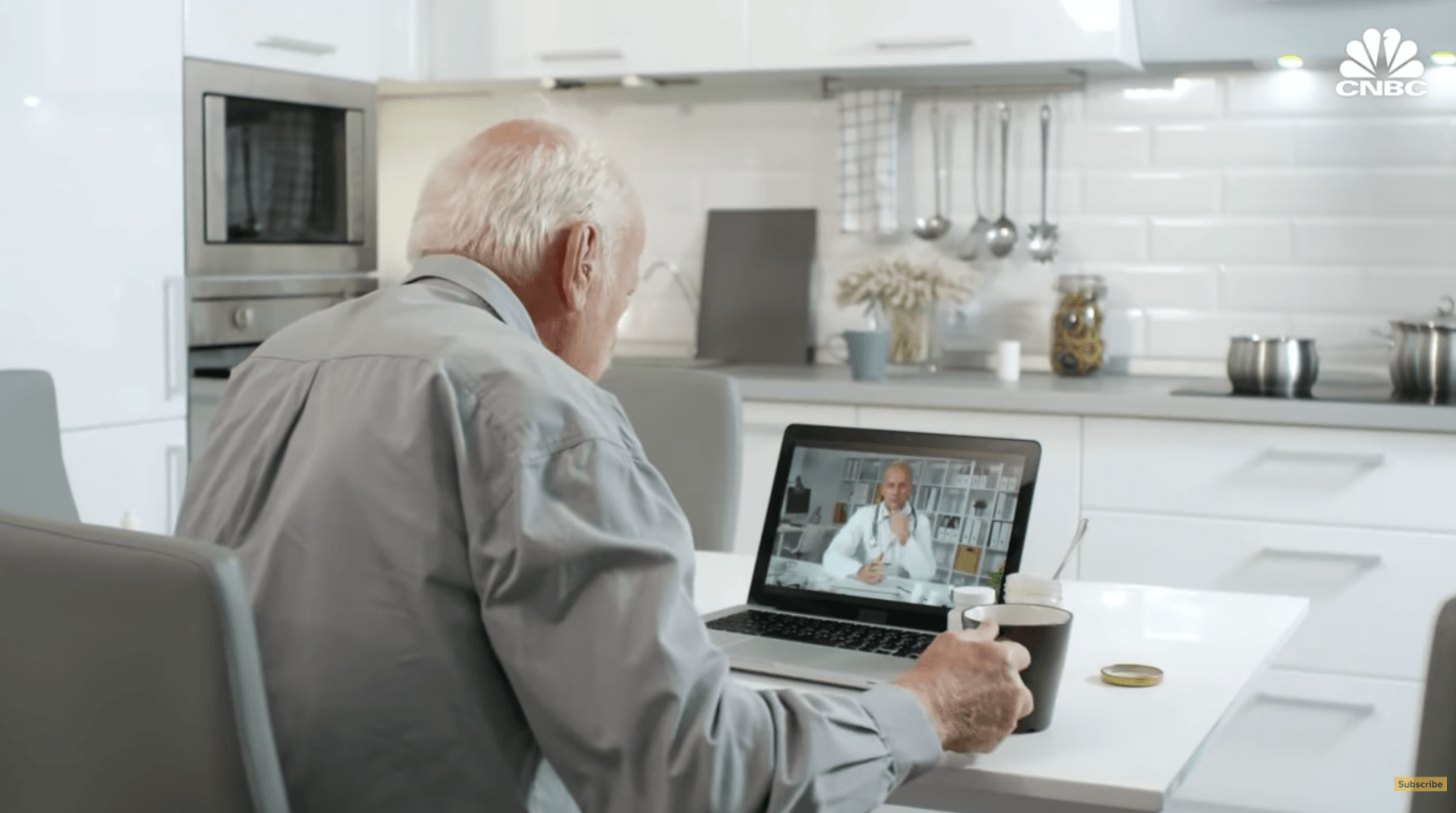
The weakness of the present healthcare system revealed by the Covid-19 crisis, along with the rise in chronic diseases associated with lifestyle changes and a rapidly aging population worldwide will shape the future of healthcare. Next-Generation Research Analyst Dr. Damien Ng took a close look at recent developments in digital healthcare, genomics, and extended longevity.

The COVID-19 pandemic has affected many elderly from receiving proper care. It has further highlighted problems faced by the elderly with dementia and chronic diseases
In this video presented by The Economist, watch how COVID-19 pandemic has impacted the elderly and how we can strive to improve the efficiency for elderly and chronic care with the rise of remote patient monitoring technology.
Telemedicine termed a 'silver lining' of the coronavirus pandemic. This time, it might just be true.
Telehealth use surged from 8% of Americans in December to 29% in May as primary care, mental health and specialists turned to remote care out of necessity during the COVID-19 pandemic, according to a UnitedHealth Group report.
Cleveland Clinic in Ohio predicts within 5 years, half of the outpatient visits in the U.S. will be virtual. Dr. Jessica Bender, clinical instructor of medicine at University of Washington states "After the pandemic is over, Telehealth will be here to stay and people won't want to go back to only in-person visits. People will want the option of telehealth visits as well. This cannot replace the entire healthcare system as people will still need to come in for their pap smears and exams, but I think people will find a preference for this. They won't have to take off a day from work or free buses to travel to the doctor's office or find child care."